|
The Causes
of Altitude Sickness
 The
percentage of oxygen in the atmosphere at sea level is about
21% and the barometric pressure is around 760 mmHg (1 bar).
As altitude increases, the percentage remains the same but
the number of oxygen molecules per breath is reduced. The
percentage of oxygen in the atmosphere at sea level is about
21% and the barometric pressure is around 760 mmHg (1 bar).
As altitude increases, the percentage remains the same but
the number of oxygen molecules per breath is reduced.
At 3,600 metres (12,000 feet) the barometric pressure is only
about 480 mmHg (0.63 bar), so there are roughly 40% fewer
oxygen molecules per breath so the body must adjust to having
less oxygen.
In addition,
high altitude and lower air pressure causes fluid to leak
from the capillaries in both the lungs and the brain which
can lead to fluid build-up. Continuing on to higher altitude
without proper acclimatisation can lead to the potentially
serious, even life-threatening altitude sickness.
 Acclimatisation Acclimatisation
The main
cause of altitude sickness is going too high too quickly.
Given enough time, your body will adapt to the decrease in
oxygen at a specific altitude. This process is known as acclimatisation
and generally takes one to three days at any given altitude,
e.g. if you climb to 3,000 metres and spend several days at
that altitude, your body will acclimatise to 3,000 metres.
If you then climb to 5,000 metres your body has to acclimatise
once again.
Several
changes take place in the body which enable it to cope with
decreased oxygen:
- The depth
of respiration increases.
- The body
produces more red blood cells to carry oxygen.
- Pressure
in pulmonary capillaries is increased, "forcing" blood into
parts of the lung which are not normally used when breathing
at sea level.
- The body
produces more of a particular enzyme that causes the release
of oxygen from haemoglobin to the body tissues.
Please
Note: There is NO substitute for proper acclimatisation!!
For
further information on the drugs used in mountain sickness
go to the Mountain Medicines page.
Cheyne-Stokes
Respirations
 Above
3,000 metres (10,000 feet) most people experience a periodic
breathing during sleep known as Cheyne-Stokes Respirations.
The pattern begins with a few shallow breaths and increases
to deep sighing respirations then falls off rapidly even ceasing
entirely for a few seconds and then the shallow breaths begin
again. Above
3,000 metres (10,000 feet) most people experience a periodic
breathing during sleep known as Cheyne-Stokes Respirations.
The pattern begins with a few shallow breaths and increases
to deep sighing respirations then falls off rapidly even ceasing
entirely for a few seconds and then the shallow breaths begin
again.
During the period when breathing stops the person often becomes
restless and may wake with a sudden feeling of suffocation.
This can disturb sleeping patterns, exhausting the climber.
This type of breathing is not considered abnormal at high
altitudes. Acetazolamide is helpful in relieving
this periodic breathing.
Acute
Mountain Sickness (AMS)
AMS is very
common at high altitude. At over 3,000 metres (10,000 feet)
75% of people will have mild symptoms. The occurrence of AMS
is dependent upon the elevation, the rate of ascent, and individual
susceptibility. Many people will experience mild AMS during
the acclimatisation process. The symptoms usually start 12
to 24 hours after arrival at altitude and begin to decrease
in severity around the third day.
 The
symptoms of Mild AMS include: The
symptoms of Mild AMS include:
- Headache
- Nausea
& Dizziness
- Loss
of appetite
- Fatigue
- Shortness
of breath
- Disturbed
sleep
- General
feeling of malaise
Symptoms
tend to be worse at night and when respiratory drive is decreased.
Mild AMS does not interfere with normal activity and symptoms
generally subside within two to four days as the body acclimatises.
As long as symptoms are mild, and only a nuisance, ascent
can continue at a moderate rate. When hiking, it is essential
that you communicate any symptoms of illness immediately to
others on your trip.
Moderate
AMS
The signs and symptoms of Moderate
AMS include:-
- Severe
headache that is not relieved by medication
- Nausea
and vomiting, increasing weakness and fatigue
- Shortness
of breath
- Decreased
co-ordination (ataxia).
|
|
 Normal
activity is difficult, although the person may still be able
to walk on their own. At this stage, only advanced medications
or descent can reverse the problem. Descending only 300 metres
(1,000 feet) will result in some improvement, and twenty four
hours at the lower altitude will result in a significant improvement. Normal
activity is difficult, although the person may still be able
to walk on their own. At this stage, only advanced medications
or descent can reverse the problem. Descending only 300 metres
(1,000 feet) will result in some improvement, and twenty four
hours at the lower altitude will result in a significant improvement.
The person should remain at lower altitude until all the symptoms
have subsided (up to 3 days). At this point, the person has
become acclimatised to that altitude and can begin ascending
again.
The best
test for moderate AMS is to have the person walk a straight
line heel to toe just like a sobriety test. A person with
ataxia would be unable to walk a straight line. This is a
clear indication that an immediate descent is required. It
is important to get the person to descend before the ataxia
reaches the point where they cannot walk on their own (which
would necessitate a stretcher evacuation).
 Severe
AMS Severe
AMS
Severe AMS
results in an increase in the severity of the aforementioned
symptoms including: Ÿ Shortness of breath at rest, Ÿ Inability
to walk, Ÿ Decreasing mental status, Ÿ Fluid build-up in the
lungs, Severe AMS requires immediate descent of around 600
metres (2,000 feet) to a lower altitude.
There are
two serious conditions associated with severe altitude sickness;
High Altitude Cerebral Oedema (HACO) and High Altitude Pulmonary
Oedema (HAPO). Both of these happen less frequently, especially
to those who are properly acclimatised. But, when they do
occur, it is usually in people going too high too fast or
going very high and staying there. In both cases the lack
of oxygen results in leakage of fluid through the capillary
walls into either the lungs or the brain.
High
Altitude Pulmonary Oedema (HAPO)
 |
Symptoms
of HAPO include:-
-
Shortness
of breath at rest
-
Tightness
in the chest, and a persistent cough bringing up
white, watery, or frothy fluid
-
Marked
fatigue and weakness
-
A
feeling of impending suffocation at night
-
Confusion,
and irrational behaviour
|
 HAPO
results from fluid build up in the lungs. This fluid prevents
effective oxygen exchange. As the condition becomes more severe,
the level of oxygen in the bloodstream decreases, which leads
to cyanosis, impaired cerebral function, and death. HAPO
results from fluid build up in the lungs. This fluid prevents
effective oxygen exchange. As the condition becomes more severe,
the level of oxygen in the bloodstream decreases, which leads
to cyanosis, impaired cerebral function, and death.
Sometimes HAPO is referred to as HAPE. They are both the same.
The difference is because of the different American spelling
(edema)

Confusion,
and irrational behaviour are signs that insufficient oxygen
is reaching the brain. One of the methods for testing yourself
for HAPO is to check your recovery time after exertion.
In cases of HAPO, immediate descent of around 600 metres (2,000
feet) is a necessary life-saving measure. Anyone suffering
from HAPO must also be evacuated to a medical facility for
proper follow-up treatment.
 Have
you, or someone you know, ever suffered from HAPO or HAPE
(high altitude pulmonary oedema/edema)? Then join the "International
HAPE Database" a registry of previous HAPE sufferers
worldwide who might consider participating in future research
studies. Have
you, or someone you know, ever suffered from HAPO or HAPE
(high altitude pulmonary oedema/edema)? Then join the "International
HAPE Database" a registry of previous HAPE sufferers
worldwide who might consider participating in future research
studies.
 High
Altitude Cerebral Oedema (HACO/HACE) High
Altitude Cerebral Oedema (HACO/HACE)
HACO is
the result of the swelling of brain tissue from fluid leakage.
Symptoms
of HACO include:-
 It
generally occurs after a week or more at high altitude. Severe
instances can lead to death if not treated quickly. Immediate
descent of around 600 metres (2,000 feet) is a necessary lifesaving
measure. It
generally occurs after a week or more at high altitude. Severe
instances can lead to death if not treated quickly. Immediate
descent of around 600 metres (2,000 feet) is a necessary lifesaving
measure.
There are some medications that may be used for treatment
in the field, but these require proper training in their use.
Anyone suffering
from HACO must be evacuated to a medical facility for follow-up
treatment.
Prevention
of Altitude Sickness
This involves
proper acclimatisation and the possible use of medications.
|
Some
basic guidelines for the prevention of AMS:-
|
 If
possible, don't fly or drive to high altitude. Start
below 3,000 metres (10,000 feet) and walk up. If
possible, don't fly or drive to high altitude. Start
below 3,000 metres (10,000 feet) and walk up.
- If
you do fly or drive, do not overexert yourself or
move higher for the first 24 hours.
- If
you go above 3,000 metres (10,000 feet), only increase
your altitude by 300 metres (1,000 feet) per day,
and for every 900 metres (3,000 feet) of elevation
gained, take a rest day to acclimatise.
- Climb
high and sleep low! You can climb more than 300 metres
(1,000 feet) in a day as long as you come back down
and sleep at a lower altitude.
- If
you begin to show symptoms of moderate altitude sickness,
don't go higher until symptoms decrease.
- If
symptoms increase, go down, down, down!
- Keep
in mind that different people will acclimatise at
different rates. Make sure everyone in your party
is properly acclimatised before going any higher.
- Stay
properly hydrated. Acclimatisation is often accompanied
by fluid loss, so you need to drink lots of fluids
to remain properly hydrated (at least four to six
litres per day). Urine output should be copious and
clear to pale yellow.
- Take
it easy and don't overexert yourself when you first
get up to altitude. But, light activity during the
day is better than sleeping because respiration decreases
during sleep, exacerbating the symptoms.
- Avoid
tobacco, alcohol and other depressant drugs including,
barbiturates, tranquillisers, sleeping pills and opiates
such as dihydrocodeine. These further decrease the
respiratory drive during sleep resulting in a worsening
of symptoms.
- Eat
a high calorie diet while at altitude.
- Remember:
Acclimatisation is inhibited by overexertion, dehydration,
and alcohol.
|
Please
Note: There is NO substitute for proper acclimatisation!!
Preventative
Medications
Acetazolamide
(Diamox): This is the most tried and tested drug for altitude
sickness prevention and treatment. Unlike dexamethasone (below)
this drug does not mask the symptoms but actually treats the
problem. It seems to works by increasing the amount of alkali
(bicarbonate) excreted in the urine, making the blood more
acidic. Acidifying the blood drives the ventilation, which
is the cornerstone of acclimatisation.
For prevention, 125 to 250mg twice daily starting one or two
days before and continuing for three days once the highest
altitude is reached, is effective. Blood concentrations of
acetazolamide peak between one to four hours after administration
of the tablets.
 Studies
have shown that prophylactic administration of acetazolamide
at a dose of 250mg every eight to twelve hours before and
during rapid ascent to altitude results in fewer and/or less
severe symptoms (such as headache, nausea, shortness of breath,
dizziness, drowsiness, and fatigue) of acute mountain sickness
(AMS). Pulmonary function is greater both in subjects with
mild AMS and asymptomatic subjects. The treated climbers also
had less difficulty in sleeping. Studies
have shown that prophylactic administration of acetazolamide
at a dose of 250mg every eight to twelve hours before and
during rapid ascent to altitude results in fewer and/or less
severe symptoms (such as headache, nausea, shortness of breath,
dizziness, drowsiness, and fatigue) of acute mountain sickness
(AMS). Pulmonary function is greater both in subjects with
mild AMS and asymptomatic subjects. The treated climbers also
had less difficulty in sleeping.
Gradual
ascent is always desirable to try to avoid acute mountain
sickness but if rapid ascent is undertaken and actazolamide
is used, it should be noted that such use does not obviate
the need for a prompt descent if severe forms of high altitude
sickness occur, i.e. pulmonary or cerebral oedema.
Side
effects of acetazolamide include: an uncomfortable tingling
of the fingers, toes and face carbonated drinks tasting flat;
excessive urination; and rarely, blurring of vision.
On
most treks, gradual ascent is possible and prophylaxis tends
to be discouraged. Certainly if trekkers do develop headache
and nausea or the other symptoms of AMS, then treatment with
acetazolamide is fine. The treatment dosage is 250 mg twice
a day for about three days.
A trial
course is recommended before going to a remote location where
a severe allergic reaction could prove difficult to treat
if it occurred.
Dexamethasone (a steroid) is a drug that decreases
brain and other swelling reversing the effects of AMS. The
dose is typically 4 mg twice a day for a few days starting
with the ascent. This prevents most of the symptoms of altitude
illness from developing.
WARNING:
Dexamethasone is a powerful drug and should be used with caution
and only on the advice of a physician and should only be used
to aid acclimatisation by sufficiently qualified persons or
those with the necessary experience of its use.
For
further information on drugs to treat mountain sickness
go to the Mountain Medicines page.
 Treatment
of AMS Treatment
of AMS
The only
cure for mountain sickness is either acclimatisation or descent.
Symptoms
of Mild AMS can be treated with pain killers for headache,
acetazolamide and dexamethasone. These help to reduce
the severity of the symptoms, but remember, reducing the symptoms
is not curing the problem and could even exacerbate the problem
by masking other symptoms.
Acetazolamide
allows you to breathe faster so that you metabolise more oxygen,
thereby minimising the symptoms caused by poor oxygenation
which is especially helpful at night when the respiratory
drive is decreased.
Acetazolamide may be obtained on prescription in the UK from
Doctor
Fox
Dexamethasone: This powerful steroid drug can be life
saving in people with HACO (HACE), and works by decreasing
swelling and reducing the pressure in the skull. The dosage
is 4 mg three times per day, and obvious improvement usually
occurs within about six hours. This drug "buys time" especially
at night when it may be problematic to descend. Descent should
be carried out the next day. It is unwise to ascend while
taking dexamethasone: unlike diamox this drug only masks the
symptoms.
 Dexamethasone
can be highly effective: many people who are lethargic or
even in coma will improve significantly after tablets or an
injection, and may even be able to descend with assistance.
Many pilgrims at the annual festival at Gosainkunda lake in
Nepal suffer from HACO following a rapid rate of ascent, and
respond remarkably well to dexamethasone. Dexamethasone
can be highly effective: many people who are lethargic or
even in coma will improve significantly after tablets or an
injection, and may even be able to descend with assistance.
Many pilgrims at the annual festival at Gosainkunda lake in
Nepal suffer from HACO following a rapid rate of ascent, and
respond remarkably well to dexamethasone.
Mountain climbers also sometimes carry this drug to prevent
or treat AMS. It needs to be used cautiously, because it can
cause stomach irritation, euphoria or depression.
It
may be a good idea to pack this drug for a high altitude trek
for emergency usage in the event of HACO In people allergic
to sulpha drugs (and therefore unable to take diamox) dexamethasone
can also be used for prevention: 4 mg twice a day for about
three days may be sufficient.
Other
Medicines used for treating Altitude Sickness include:-
 Ibuprofen
which is effective in relieving symptoms & altitude induced
headache. Ibuprofen
which is effective in relieving symptoms & altitude induced
headache.
Nifedipine:
This drug is usually used to treat high blood pressure. It
rapidly decreases pulmonary artery pressure and also seems
able to decrease the narrowing in the pulmonary artery caused
by low oxygen levels, thereby improving oxygen transfer. It
can therefore be used to treat HAPO, though unfortunately
its effectiveness is not anywhere as dramatic that of dexamethasone
in HACO. The dosage is 20mg of long acting nifedipine, six
to eight hourly.
Nifedipine can cause a sudden lowering of blood pressure so
the patient has to be warned to get up slowly from a sitting
or reclining position. It has also been used in the same dosage
to prevent HAPO in people with a past history of this disease.
Frusemide
may clear the lungs of water in HAPO and reverse the suppression
of urine brought on by altitude. However, Frusemide can also
lead to collapse from low volume shock if the victim is already
dehydrated. Treatment dosage is 120mg daily.
Breathing
· 100% Oxygen also reduces the effects of altitude sickness.
The
Gamow Bag
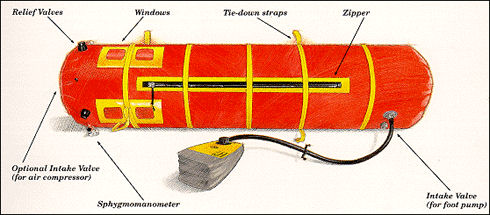
 This
clever invention has revolutionised field treatment of altitude
sickness. The bag is composed of a sealed chamber with a pump. This
clever invention has revolutionised field treatment of altitude
sickness. The bag is composed of a sealed chamber with a pump.
The casualty is placed inside the bag and it is inflated by
pumping it full of air effectively increasing the concentration
of oxygen and therefore simulating a descent to lower altitude.
In
as little as 10 minutes the bag can create an "atmosphere"
that corresponds to that at 900 to 1,500 metres (3,000 to
5,000 feet) lower. After two hours in the bag, the person's
body chemistry will have "reset" to the lower altitude.
This acclimatisation lasts for up to 12 hours outside of the
bag which should be enough time to get them down to a lower
altitude and allow for further acclimatisation.
The
bag and pump together weigh about 6.5 kilos (15 pounds) and
are now carried on most major high altitude expeditions. Bags
can be rented for short term treks or expeditions.
|